by Comprehensive Orthopaedics | Jan 10, 2023 | Elbow, pain, Wellness
Bicep tears are common, but many people fail to realize that the pain they’re feeling is actually caused by their bicep, not their shoulder. You may not realize it, but you put a lot of strain on your shoulders when lifting weights or playing common sports like...
by Comprehensive Orthopaedics | Dec 28, 2021 | Elbow
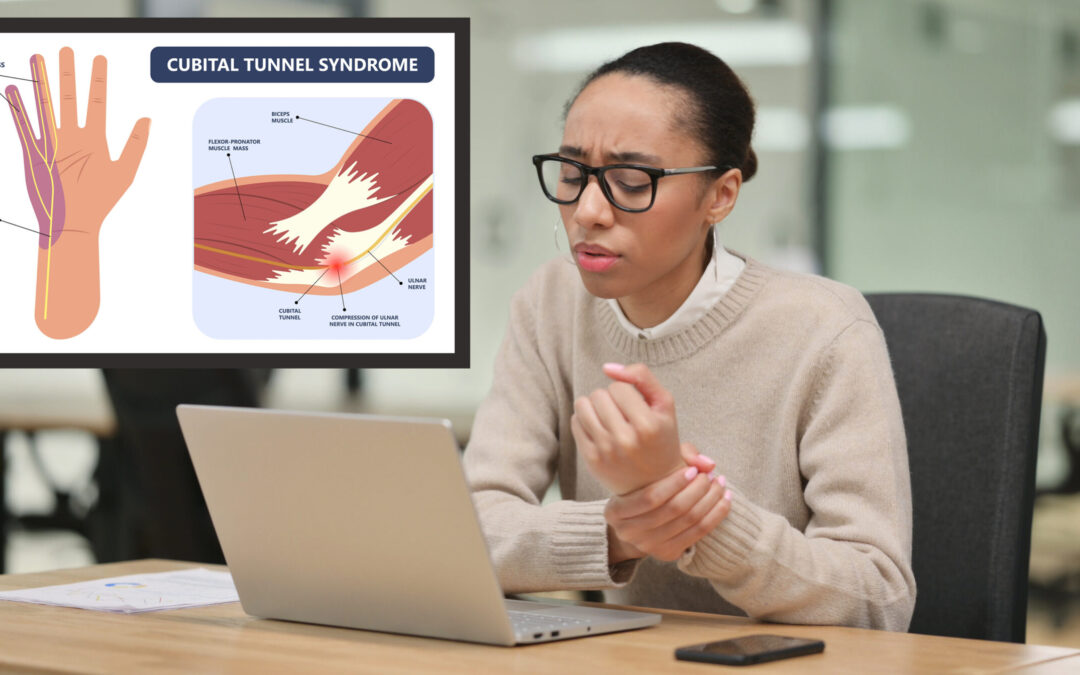
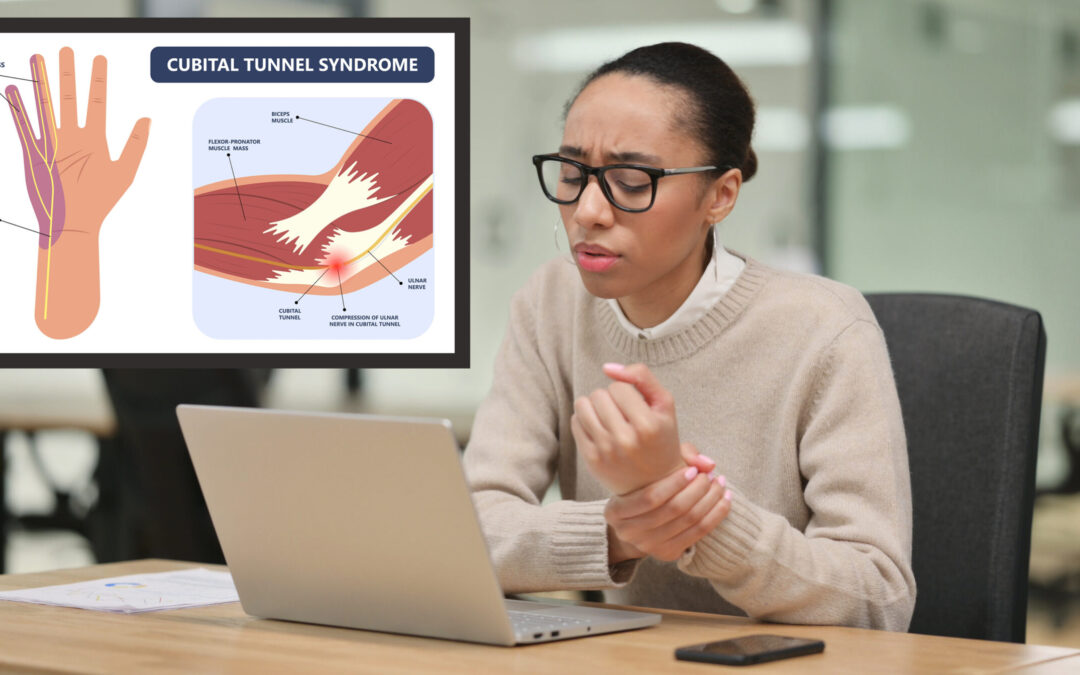
Most people have heard of carpal tunnel syndrome, but do you know about it’s lesser-known cousin, cubital tunnel syndrome? Find out how to prevent and treat the common condition. If you spend your days hunched over a computer banging on a keyboard, you’re probably...

by Comprehensive Orthopaedics | Aug 18, 2021 | anatomy, Elbow, Exercise, pain, surgery, Wellness
Tennis elbow, or lateral epicondylitis, is a painful condition of the elbow caused by overuse. Not surprisingly, playing tennis or other racquet sports can cause this condition. However, several other sports and activities besides sports can also put you at risk. ...

by Comprehensive Orthopaedics | Jun 15, 2020 | Elbow, Hand, pain, Wrist
Carpal tunnel syndrome and cubital tunnel syndrome share similar symptoms, but they are distinct conditions affecting different nerves in the elbow and wrist. If you’re experiencing pain and numbness in your fingers, you may assume you have carpal tunnel syndrome....

by Comprehensive Orthopaedics | Jun 11, 2020 | Elbow, Wellness
Don’t let elbow pain keep you from enjoying a day at the golf course. Avid golfers eagerly anticipate the start of spring so they can once again head to the golf course and enjoy an afternoon in the sun. Yet as you inspect your clubs to make sure they’re in top shape...

by Comprehensive Orthopaedics | Jul 30, 2019 | Anti-aging, Elbow, Hand, pain, Wellness
MONDAY, July 29, 2019 (HealthDay News) — Repetitive strain injury (RSI) can affect anyone who uses his or her hands a lot and repeats the same movements over and over again. It can develop whether you’re working at a computer all day or spending hours of...