by Comprehensive Orthopaedics | Aug 30, 2021 | pain, Spine
THURSDAY, Aug. 26, 2021 (HealthDay News) — A new approach to spinal cord stimulation may drastically reduce chronic back pain, a small pilot study suggests. The study, of 20 patients with stubborn low back pain, tested the effects of implanting electrodes near...

by Comprehensive Orthopaedics | Aug 24, 2021 | Anti-aging, Exercise, pain, Wellness
Feeling achy and stiff in the morning? Try these seven techniques to ease into the day. Nothing is more restorative than a good night’s sleep. You wake up refreshed and ready to take on a new day. Yet, for some people, the early morning hours bring unwelcome neck and...

by Comprehensive Orthopaedics | Aug 18, 2021 | anatomy, Elbow, Exercise, pain, surgery, Wellness
Tennis elbow, or lateral epicondylitis, is a painful condition of the elbow caused by overuse. Not surprisingly, playing tennis or other racquet sports can cause this condition. However, several other sports and activities besides sports can also put you at risk. ...

by Comprehensive Orthopaedics | Aug 16, 2021 | Hip, pain, Wellness
Arthritis isn’t the only cause of hip pain. Find out which condition may be causing your discomfort — and how to treat it. Hip pain doesn’t only affect older adults — stiffness and pain in this joint can strike younger people, too. Although osteoarthritis ranks high...
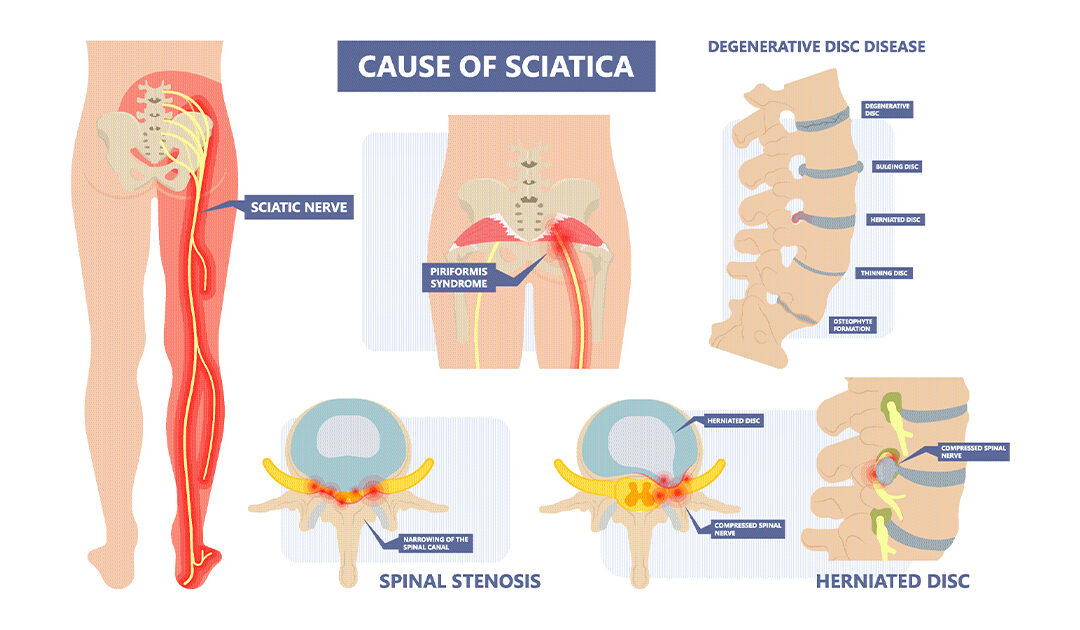
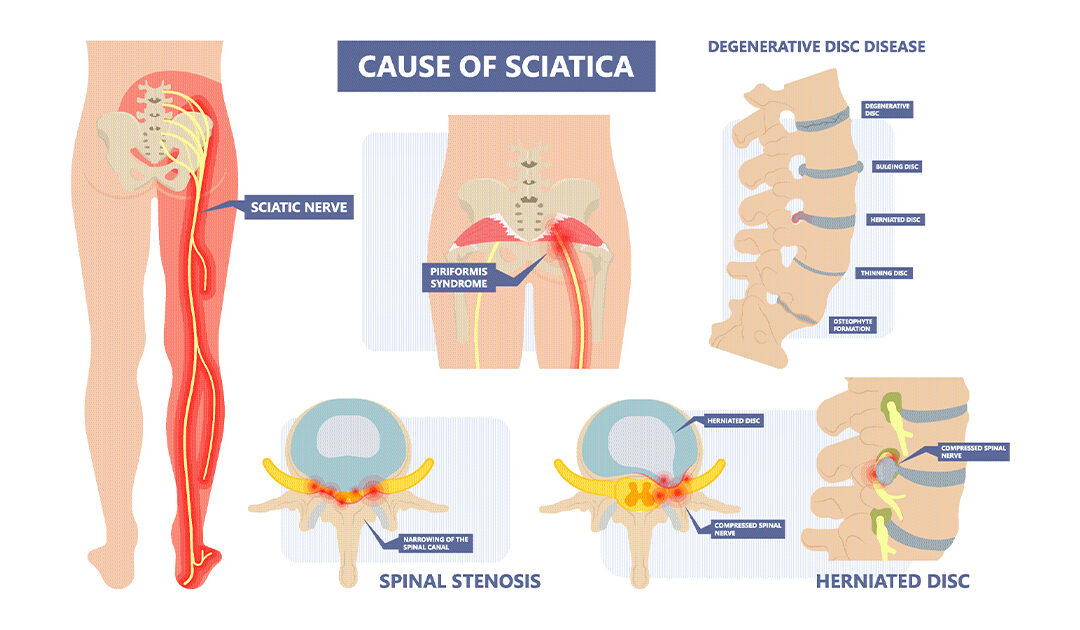
by Comprehensive Orthopaedics | Aug 2, 2021 | Spine
There’s much Americans may disagree on, but many share one thing in common: chronic pain. More than half of U.S. adults suffer from pain, with backs and legs the most common sources, according to researchers from the U.S. Centers for Disease Control and...