by Comprehensive Orthopaedics | Apr 18, 2018 | Anti-aging, arthritis, Exercise, Wellness
With aging often comes worry about falls and the bone fractures they cause. Now, a panel of U.S. experts has new advice on what helps and what doesn’t when it comes to staying upright. For starters, get off the sofa. And don’t rely on vitamin D to keep you...

by Comprehensive Orthopaedics | Apr 18, 2018 | Anti-aging, Exercise, Wellness
Is arthritis pain getting in the way of your fitness plans? That need not be the case. In fact, physical activity can be vital to your continued mobility. Osteoarthritis is a joint disease that affects about 27 million Americans — most often in the knees and...
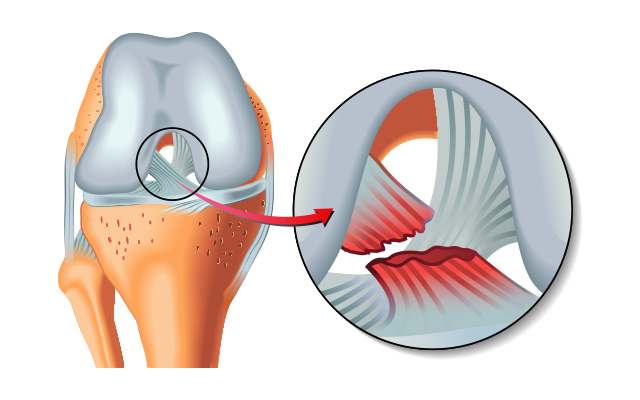
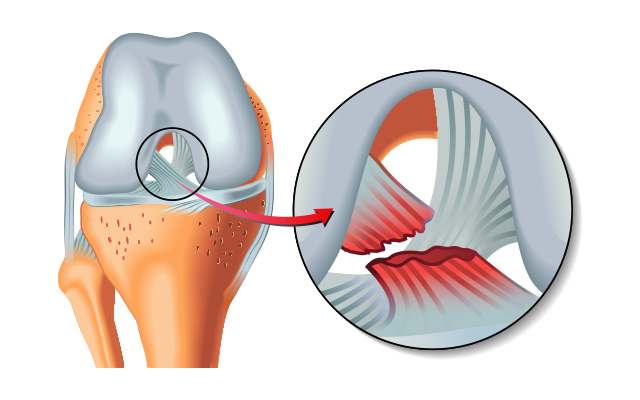
by Comprehensive Orthopaedics | Apr 16, 2018 | Knee, pain, surgery, Wellness
Professional athletes’ speedy recoveries from injuries have nothing to do with superhuman abilities. Instead, it’s all about proper preparation and planning. It’s no surprise that professional athletes tend to be in much better shape than those of us who don’t play...

by Comprehensive Orthopaedics | Apr 11, 2018 | Anti-aging, pain, Wellness
When you’re dealing with an injury involving bones, muscles, or joints, the first healthcare professionals who probably come to mind are orthopedic surgeons or sports medicine doctors. These are the physicians we most often turn to when it’s the musculoskeletal system...

by Comprehensive Orthopaedics | Apr 11, 2018 | anatomy, Anti-aging, arthritis, Hand, pain
If you have stiff, aching fingers and hands, you’re not alone — a new study reports that 40 percent of people will be affected by the pain of arthritis in at least one hand. The rate seen in the new research is “just slightly below the percentage of...