by Comprehensive Orthopaedics | Mar 29, 2017 | Anti-aging, arthritis
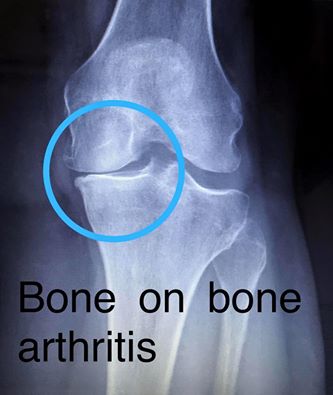
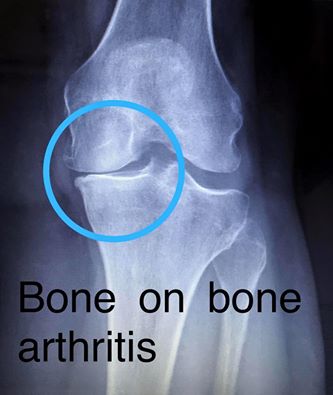
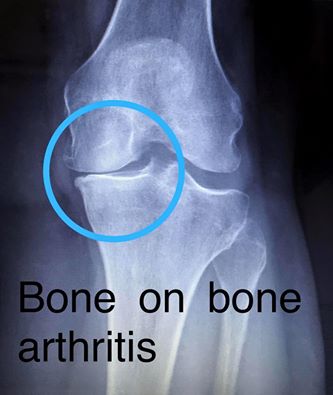
Arthritis is expanding its grip on Americans, with 24 million adults limited in their everyday activities because of the debilitating joint disease, U.S. health officials say. Overall, 54 million adults — or one in four — report an arthritis diagnosis. And...

by Comprehensive Orthopaedics | Mar 23, 2017 | pain, Spine
What is a whiplash? Whiplash is an injury to your neck. It is caused by your neck bending forcibly forward and then backward, or vice versa. The injury, which is poorly understood, usually involves the muscles, discs, nerves, and tendons in your neck. What causes a...

by Comprehensive Orthopaedics | Mar 14, 2017 | Wellness
If you’re trying to determine the difference between an MD and a DO, you almost certainly fit into one of two categories. You’re either a student considering a career in medicine or a patient wondering what exactly the difference is. What is an MD? When most people...

by Comprehensive Orthopaedics | Mar 14, 2017 | Anti-aging, arthritis, Wellness
Arthritis is expanding its grip on Americans, with 24 million adults limited in their everyday activities because of the debilitating joint disease, U.S. health officials say. Overall, 54 million adults — or one in four — report an arthritis diagnosis. And...

by Comprehensive Orthopaedics | Mar 1, 2017 | Ankle, Elbow, Hip, Knee, pain, Shoulder, Wellness
Exercise is good for the body and with the proper precautions, sports injuries can often be prevented. The quality of protective equipment – padding, helmets, shoes, mouth guards – have helped to improve the safety in sports. But, you can still be...