by Comprehensive Orthopaedics | Jun 23, 2020 | Spine, Wellness
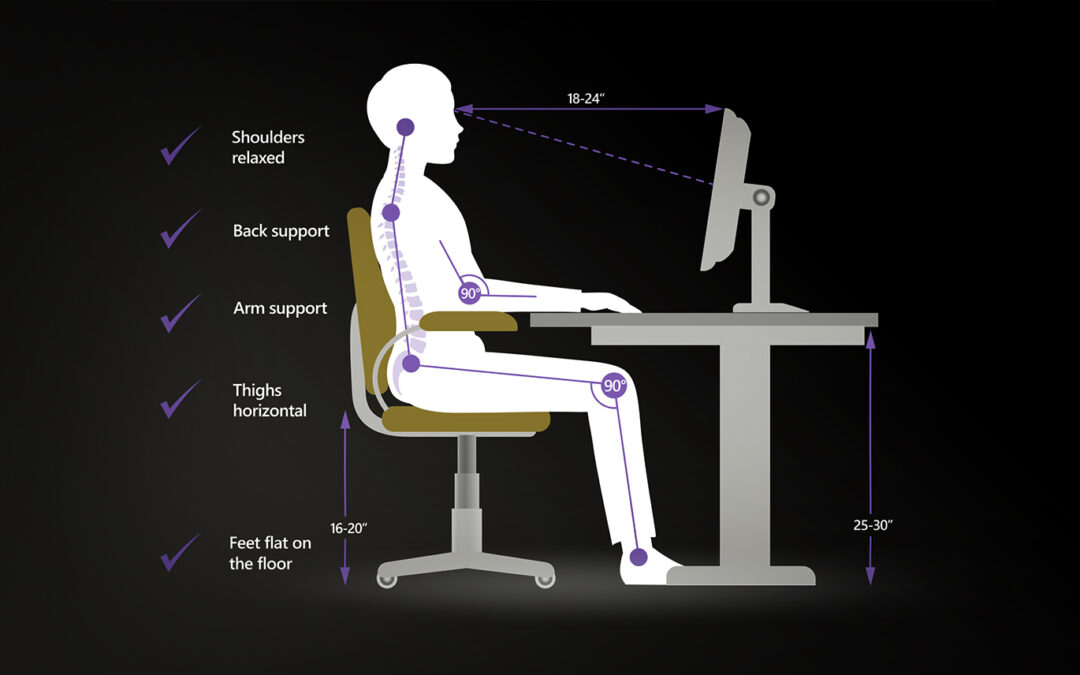
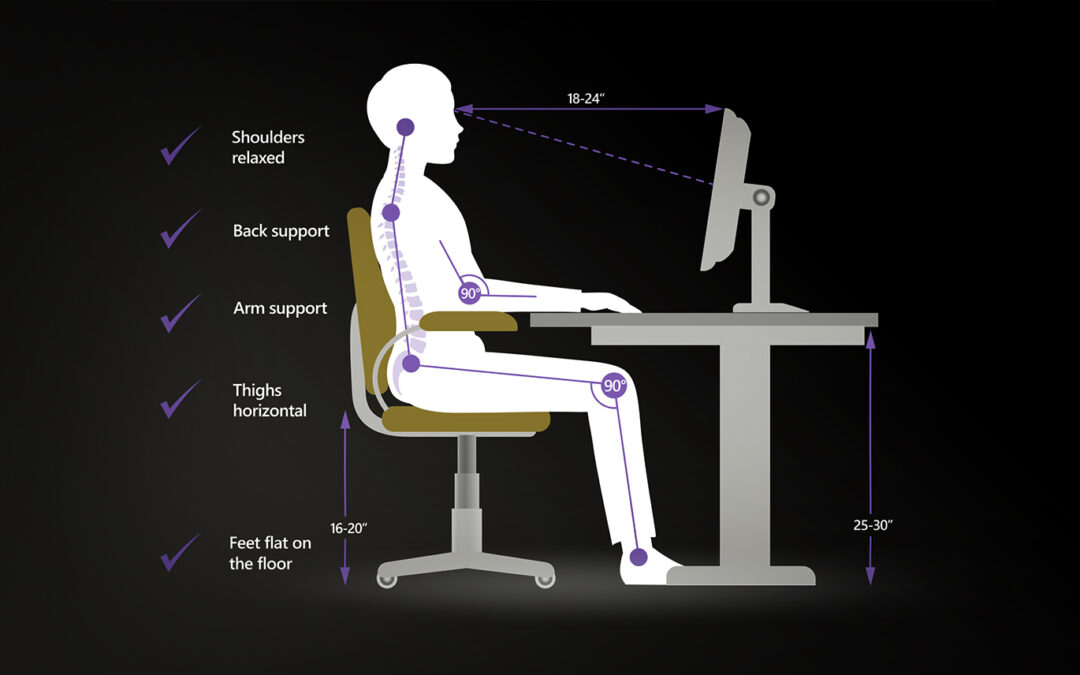
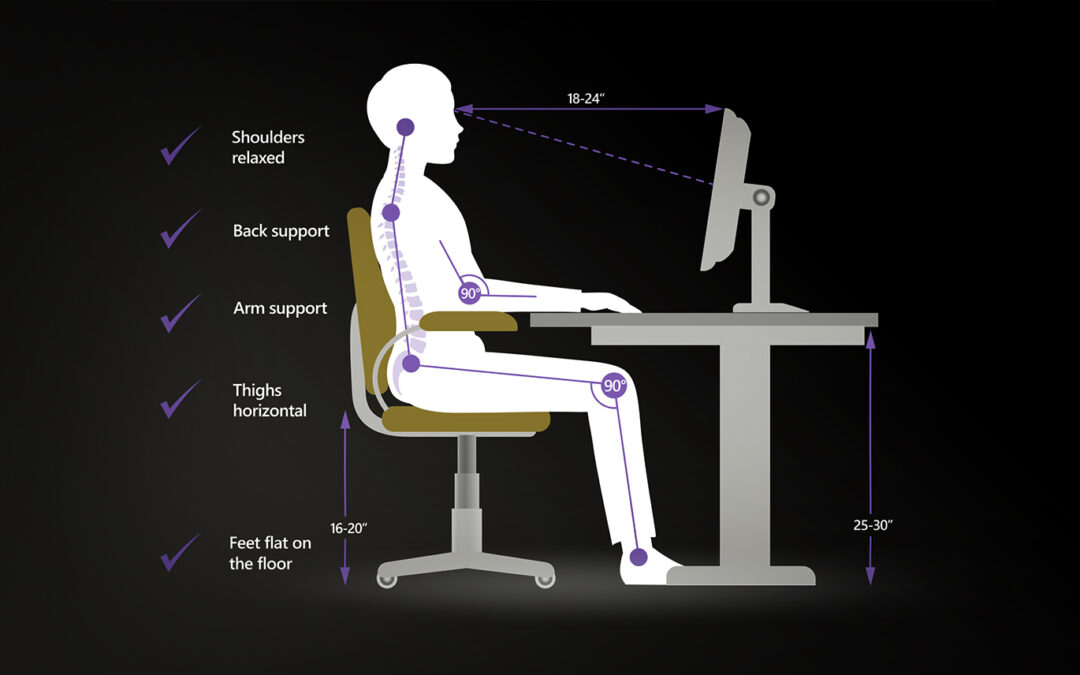
FRIDAY, June 19, 2020 (HealthDay News) — If you’re working from home because of the coronavirus pandemic and expect to keep doing so, you need to be sure your work station is set up properly, an orthopedic specialist says. You also need to take regular...

by Comprehensive Orthopaedics | Jun 18, 2020 | pain, Spine, surgery, Wellness
TUESDAY, June 16, 2020 (HealthDay News) — Patients with lower back problems often worry about how much time they’ll need to recover if they have surgery. A new study finds similar results for two common minimally invasive spine procedures. Surgery may be...

by Comprehensive Orthopaedics | Jun 15, 2020 | Elbow, Hand, pain, Wrist
Carpal tunnel syndrome and cubital tunnel syndrome share similar symptoms, but they are distinct conditions affecting different nerves in the elbow and wrist. If you’re experiencing pain and numbness in your fingers, you may assume you have carpal tunnel syndrome....

by Comprehensive Orthopaedics | Jun 11, 2020 | Elbow, Wellness
Don’t let elbow pain keep you from enjoying a day at the golf course. Avid golfers eagerly anticipate the start of spring so they can once again head to the golf course and enjoy an afternoon in the sun. Yet as you inspect your clubs to make sure they’re in top shape...